Teona Shulaia2, Natalia Kiladze1,2, Agata Bulinska3, Ljubomyr Abrahamovych4
1Tbilisi State Medical University, Dermato-venerology department;
2Medical Center “Marjani”, Tbilisi, Georgia;
3School of Medicine, The University of Queensland, Brisbane,
4Danylo Halytsky Lviv National Medical University
Introduction. The need for research of acral melanocytic tumors of the skin is primarily concerned with the study of acral lentiginous melanoma which has variable frequency in different populations worldwide. Structurally accounting is not more than 10.0 % of all forms of skin cancer, melanoma causes 80.0 % of deaths attributable to this group of tumors [1]. The lack of alertness in identifying of the background for the development of melanoma as well as late detection of its early stages of development in most cases leads to its late diagnosis and high mortality of patients. The accuracy of visual diagnosis of melanocytic tumors of the skin depends on the specialization of doctors and the frequency of occurrence of these tumors in their daily practice. However, currently in the literature there is fairly complete information on different properties of melanoma, as well as tumors of similar histogenesis such as nevi, still are not resolved some issues of the histogenesis, classification and terminology of these tumors; unknown are details of their biological essence that determines the diversity in the clinical and morphological manifestations, there is no clear differential criteria for the diagnosis of precursors of melanoma [2]. It is well known that some varieties of nevi may be related to the group of precursors of melanoma, therefore, require careful and in-depth study as a background of the disease threatening for the occurrence of malignant melanoma.
Acral nevi represent melanocytic proliferation in the palms and soles. They are found in approximately 4.0 % of people with white skin, more often may be found in coloured skin, and represent as a striped broun spot on the slin of palm and soles or under the nail plate. The term sometimes is discussable because some authors refer to acral nevi lesion on both volar and dorsal surfaces, the other ones limit this term only to acral volar surfaces. In highly pigmented acral nevi the pigment melanin is often observed in the stratum corneum of the epidermis in the form of stripe-like extracellular structures between horny scales, which tend to exfoliate with them. These characteristics should not be considered as a manifestation of the malignant properties of tumors, as atypical melanocytes are not detected and acral nevi are benign structures, but their location in frequently traumatized areas require attention, thus it is estimated that acral lentigious melanoma in white population represents about 10.0 % of all cutaneous melanomas, being the most prevalent form of this tumor in non-caucatian population [8]. Pigmented acral lesions often represent a diagnostic challenge, in which dermoscopy carries an important role as it allows the identification of specific patterns of benignancy or malignancy. Dermatoscopic diagnosis of acral tumors is based on the same principles as in other localizations but has its own characteristic features associated with structural features of smooth skin (the linearity of the skin pattern, the abundance of sweat glands and absence of hair follicles).
Purpose of the study. The primary aim of our study was to investigate the dermoscopic features of 306 acral melanocytic nevi, to determine the most common patterns and to trace their connection with development of acral lentiginous melanoma.
Materials and methods. We retrieved digital images of 306 acral melanocytic lesions in 117 patients (45 males and 72 females; age from 4 up to 82 years), among them were detected 5 acral melanomas in 5 patients (2 males and 3 females; mean age 65 years). All studied patient were Caucasians. Other demographic indexes such as Fitzpatrick skin type, number and site of acral nevi were collected for each patient. For each patient was collected data of the predominant body pattern of the nevi, the number of volar lesions, the location and diameter of each volar lesion and dermoscopic patterns. Lesions located on dorsal areas were excluded. Locations on the palms and soles were schematically divided into the following categories: thenar eminence, hypothenar eminence, volar aspect of digits, and rest of the palm and subungual location. Digital dermoscopic images were captured with a Sumsung Galaxy S4 digital camera equipped with a Dermlite DL3 dermoscope. All the images were jointly evaluated by the group of dermatologists (authors). The patterns were classified according to the Harald Kittler’s pattern analysis [5].
The specificity of this algorithm is based on 5 simple geometric structures, colors and their combinations, giving a system of clear criteria for evaluating of different types of pigmented skin tumors, including melanoma.
The majority of patients represented the 2nd skin type (62.0 %), 1st type – 32.0 % and only few cases (6.0 %) – 3rd skin type.
Benign lesions were located on the thumb eminence (12.0 %), hypothenar eminence (9.0 %), volar aspect of digits (12.0 %), rest of the soles (63.0 %) and subungual location (4.0 %).
Clinically the majority of lesions were small (less than 7 mm in diameter), flat, with brown or dark brown coloration and usually well demarcated, those slightly elevated or bigger in size had a darkerly colorated or a bit bluish center. According to the types of nevi in acral location in this study we noted practically all types. Among them only in one case was Clark nevus located on the base of a big toe.
The dermatoscopic diagnosis of acral lesions is based on the same principles as those at other locations, but because the different structure of epidermis in these two anatomical areas some dermoscopic aspects of lesions located on volar skin differ from those located on nonglabrous skin sites [3]. According to the literature the dominant dermatoscopic patterns of acral nevi are parallel lines located in the furrows [6, 7].
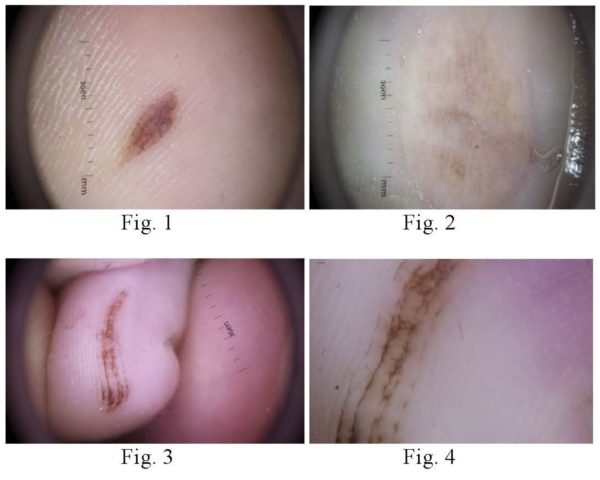
Results of the investigation ant their discussion. In our study the pattern of parallel lines located in the furrows was fixed in the majority of cases (84.0 %) and they were typical. Parallel lines were seen in furrows and in some cases on the ridges. Those, located on ridges were symmetrical and ranked. In some cases (14.0 %) located in furrows parallel lines were connected with сrossing lines, giving the impression of reticular. Such ″crossing pattern″ was most common in the areas that are subjected to pressure. As a rule in each furrow was one pigmented line, in some cases there were two, but usually these lines were composed from dots and they were not continual. Except the parallel lines where were noted other patterns. Dots, clods and the structureless pattern were seen frequently, reticular lines less often, radial lines rarely. As to distribution of dermoscopic patterns according to the anatomical site of the lesions – parallel, reticular lines and structureless pattern were more often in the nevi located on the soles in comparison with those on the fingers or volar area.
Fig. 1, 2, 3, 4. Acral nevi, dermatoscopic picture: parallel lines in the furrows are the typical pattern of acral nevi. Fig. 3, 4 The parallel lines in the furrows are connected by crosswise lines, giving an impression of reticular lines. Fig. 2 structureless pattern.
Dermatoscopy of nails pigmentation was provided with ultrasound gel for dermatoscopy. All studied nails were with longitudinal melanonychia running continuously from the lunula to the free end of the nail plate. In majority of cases were fixed light brown and grey parallel lines, they were of the similar color, located on the equal distance from each other. These lines were extending the whole length of the nail plate. Only in two cases we found structureless pattern and clods together with parallel lines, but both these cases were connected with trauma and bleeding.
The 5 acral melanomas, which were all located on the soles, were from 5 patients with skin types I (n = 1) and II (n = 4). No one of these patients recalled trauma history and noone of them could not recall whether any other lesion had been diagnosed at the site of the melanoma. One of patient did not know anything about pigment lesion and applied with claims of dryness of the skin and itching. Lesions on the skin initially appeared as a pigmented macule, then progressed to a rapidly expanding plaque with irregular, notched borders and darkly pigmented. In one case the clinical picture was described as an elevated nodular lesion located on the heel.
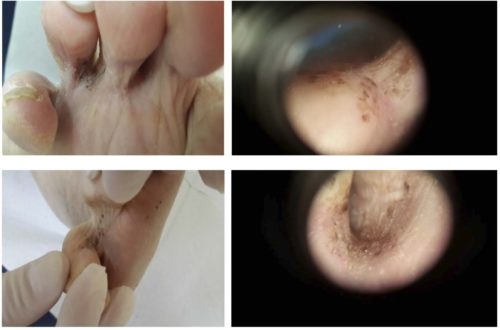
Fig. 5. In some cases the clinical picture is so specific that it does not need the dermatoscopy.
Fig. 6. Acral Melanoma. Clinical left column, dermatoscopy right column. An acral melanoma with a structureless pattern and variegate pigmentation. More than one pattern, clods and gray clods are a clue to melanoma. Histopathological diagnosis: Melanoma (> 1 mm).
The main dermatoscopic feature in all cases were parallel lines on the ridges, which in all described in the literature cases are the key sign for acral melanoma [3], especially for non-invasive ones. In all our cases as a rule these parallel lines were chaotic, asymmetrically located, their colors varied from light brown to dark, grey and black. Together with parallel lines were fixed such characteristics as the existence of more than one pattern, structureless areas with non-central location, black and grey clods distrubuted asymmetrically. All lesions were with few colors, but brownish-black and grey or grayish were the main. Only in one case with only parallel lines on the ridges, suspicious because of their gray-brown color, the pigmented lesion was removed and histologically was confirmed melanoma in situ.
According to the statistic data each year in the world are detected about 2 million patients with cancer of the skin, among them cases of melanoma account about 3.0-4.0 %, but it is one of the most aggressive tumors. The incidence of melanoma is constantly increasing among all races, and its early diagnosis is one of the most important issues in dermatooncology. Especially difficult for early diagnosis is acral melanoma – primary melanoma developed on the skin of the fingers, interdigital spaces, soles, palms, nail plates. Until now, doctors have difficulties in the differential diagnosis of melanoma, premilinary tumors and benign nevi, as there are no clear algorithms for clinical diagnosis of these groups of tumors and evaluation of the contribution of individual characteristics in making diagnostic hypotheses. Our physicians, unfortunately, still rarely use for diagnostic so powerful, simple and non-invasive method as dermatoscopy, giving a possibility for accurate and reliable determination of tumor’s parameters. In all our benign cases of acral nevi highly specific signs were parallel structures – pigmented parallel lines located in the furrows in some cases making the reticular net. Such pattern is typical for benign lesions and was described as typical in the literature [4]. For malignant pigmented lesions typical are lines located on the ridges, to distinguish the ridges from the furrows allows the presence on top of them the outlets of the sweat glands which have the appearance of a whitish, fuzzy-edged spots, arranged in the form of a chain.
Conclusions. Thus, each nosological unit of acral nevi has its particular dermatoscopic pattern that helps to differentiate between malignant and benign proliferation. Specific dermatoscopic sign of acral melanoma is the pattern of parallel ridges, while for nevi typical pattern is parallel furrows. The widespread introduction of dermoscopy into practice will enable dermatologists to diagnose melanoma in its early stages of development and to avoid unjustified removal of benign tumors.
References
- Demidov LV, Kharkevich GU. Skin melanoma. Staging, diagnostic and treatment. PMJ. 2003;11:658. (Russian)
- Chervonnaja LV. Diagnostic of skin melanocytic neoplasms [dissertation]. Moskow; 2003. (Russian)
- Argenziano G, Soyer HP. Dermoscopy of pigmented skin lesions – a valuable tool for early diagnosis of melanoma. Lancet Oncol. 2001;2(7):443-449. https://doi.org/10.1016/S1470-2045(00)00422-8
- Barquet V, Dufrechou L, Nicoletti S, Acosta MA, Magliano J, Martínez M et al. Dermoscopic Patterns of 158 Acral Me- lanocytic Nevi in a Latin American Population. Actas Dermo-Sifilograficas. 2013;104(7):586-592. https://doi.org/10.1016/j.ad.2013.01.006
- Kittler H, Rosendahl C, Cameron A, Tschandl P. Dermatoscopy. An algorithmic method based on pattern analysis. Facultas Verlags- und Buchhandels AG, Univertatsverlag, Autria, 2011.
- Miyazaki A, SaidaT, Koga H, Oguchi S, Suzuki T, Tsuchida T. Anatomical and histopathological correlates of the dermoscopic patterns seen in melanocytic nevi on the sole: a retrospective study. J Am Acad Dermatol. 2005;53:230-236. https://doi.org/10.1016/j.jaad.2005.04.045
- Saida T, Koga H. Dermoscopic patterns of acral melanocytic nevi: their variations, changes, and significance. Arch Dermatol. 2007;143:1423-1426. https://doi.org/10.1001/archderm.143.11.1423
- Fracaroli TS, Lavorato FG, Maceira JP, Barcaui C. Parallel ridge pattern on dermoscopy: observation in non-melanoma cases. An Bras Dermatol. 2013;88(4):646-648. https://doi.org/10.1590/abd1806-4841.20132058