N. Emelyanova
State Institution “L.T. Malaya National Institute of Therapy of NAMS of Ukraine”, Kharkiv
Introduction. One of the priority directions of modern dentistry is the study of pathological changes in the oral cavity in patients with somatic pathology, namely chronic obstructive pulmonary disease (COPD) [4, 8].
Today, COPD is understood as a progressive disorder of the function of external respiration associated with inflammatory reaction of the pulmonary tissue to irritation with various pathogens and gases [7]. The high prevalence and increase of COPD morbidity, the number of disabled people of working age and the severity of the prognosis make this disease one of the most urgent problems of clinical pulmonology, both in the world and in Ukraine. In recent years, mechanisms of close association of COPD with cardiovascular diseases, namely ischemic heart disease (IHD), are widely discussed, and its combination, according to various authors, occurs in more than 55% of cases [3].
Both COPD and IHD are accompanied by the development of systemic hypoxia, and against existing metabolic disorders of oxygen deficiency in the tissues of periodontal suppresses regenerative and reparative processes [1, 6, 10]. The increase in total intoxication of the body in COPD and IHD and pathogenetic therapy, which is prescribed to patients, cannot but affect the state of periodontal tissues. Consequently, pathological processes in the oral cavity and the indicated somatic pathology, together with a similar etiology, could have a mutually burdening effect [9].
Today, exfoliative cytology is very commonly used as an early diagnosis of the pathology of the tissues of the oral cavity. Clinical and experimental data suggest that relatively simple non-invasive methods of exfoliative cytology enable to study the influence of various systemic and external factors on cell parameters and cellular structures at various pathological gingival conditions [2, 5]. The most informative parameters that may appear on the background of the absence of visible clinical changes in the oral mucosa include the various cellular anomalies that occur as a result of genetic or metabolic (degenerative) disorders. Manifestations of cellular anomalies include micronuclei, binuclear, karyorhexis, carriolysis, picnosis, chromatin condensation, protrusion (the effect of a broken egg, blister, etc.), vacuolisation, and halo (koilocytosis).
Despite the fact that in the literature a considerable number of works devoted to the diagnosis and treatment of periodontal diseases in patients with both COPD and IHD, the state of gingival epithelium in these patients is practically not studied. Therefore, the above types of anomalies of cells became the subject of this study.
Study objective. To investigate the frequency and nature of gingival epitheliocyte nucleus in patients with COPD in combination with IHD.
Materials and methods. In order to determine the dental status, 239 patients who were under outpatient and inpatient treatment at the Cardiology and Pulmonology Department at the State Establishment “National Institute of Therapy named after L.T. Maloi of NAMS of Ukraine” were examined.
All patients, depending on the underlying disease, were divided into groups: the main group included 130 patients diagnosed with COPD in combination with IHD, the comparison group number 1 consisted of 38 patients diagnosed with COPD, and the comparison group number 2 -71 patients with IHD diagnosis. The control group was represented by 20 somatically healthy patients, representing by gender and age. The distribution of patients in groups is presented in Fig. 1.

Fig. 1. Distribution of the study patients by groups.
Criteria for exclusion from the study were: exacerbation of COPD; chronic heart failure of IV functional class; acute heart failure; severe heart rhythm disturbances; hormonal disorders of the thyroid gland; history of tuberculosis, pulmonary developmental defects; bronchial asthma; insulin-dependent diabetes mellitus, active inflammatory processes in the oral cavity.
Cytological and morphometric studies were performed on the scrapes of the gingival epithelium. After rinsing the oral cavity with a physiological solution, the end of the sterile dental spatula gently squeezed the contents of the surface layer of the epithelium of the attached gingival and transferred it to the slide. The smears were dried for 2-3 minutes at open air. The cytological preparations were stained by Papanicolau and studies under Micros Microscopes (Austria). To get a photo of cells, the digital camera CAM 2800 was used with light microscopy (lens x40, eyepiece x10). The frequency of cells with anomalies was determined per 1000 cells. To differentiate and correctly interpret nuclear cell anomalies, DNA-specific staining, in particular acridine, was used. The preparation was considered appropriate to study only when the cells were located in one layer. For the analysis of the micronuclei, isolated cells with continuous smooth edge of the nucleus were selected. Micronucleus was identified as a circular or oval-shaped chromatin body with a continuous smooth facet, sized of more than 1/3 of the nucleus, which is separately from the nucleus, does not refract light and has an intensity of coloration, drawing of chromatin is as in the core nucleus and is in one plane with it. Protrusions of the nucleus most often are looked like a “broken egg” in the form of a micro nucleus, which is combined with the nucleus with the bridge of the nucleoplasm.Statistical processing was performed using computer programs “SPSS 13”. The comparison of quantitative parameters was carried by Mann-Whitney test.
Study results and their discussion. The analysis of the study results showed that all patients with somatic pathology showed marked morphological changes in the epithelial cells, namely: an increase in the number of cells that had no nucleus and cells with large unevenly stained nuclei, whereas the nuclei of the epithelial cells of somatic-healthy donors were small and compact. The average frequency of cells with micronuclei in the scrap from the gingival epithelium of the control group was 2.00 (1.25; 3.00), which did not exceed the mean populations. The average values of the frequency of cells with this pathology obtained in somatic healthy individuals coincide with the literature data regarding the levels of micronuclei in the epithelial cells (the frequency of epithelial cells with micronuclei for different populations varies from 0 to 9 per 1000 cells in the absence of a pathology or the action of a number of harmful factors).
Patients with COPD in combination with ischemic heart disease (main group) showed the highest increase of this parameter (by more than 1.5 times compared with the control group), which is most likely due not only to the development of pathological processes, but also to the violation of apoptosis.
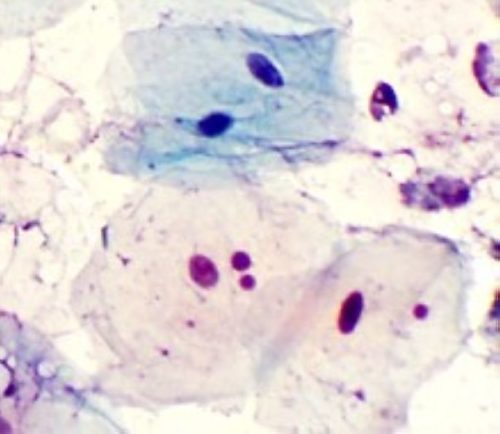
Fig. 2. Microphotography of the patient’s gingival epithelium cytogramm. An epithelial cell with microcircuits is determined. Staining by Papanicolau × 400.
As the main factors in the formation of micronuclei, they consider changing the mitotic distribution under adverse conditions, multi-polar mitosis and loss of a part of the genetic material.
In addition, patients in the main group and the comparison group number 1 (COPD) had an increased number of binuclear cells, which exceeded this value by more than 2 times not only in comparison with control, but also with group number 2 (Table 1).
Table 1
The frequency of cells with anomalies in the gingival epithelium of the examined patients
| Parameter | Group | Value |
| Micronuclei | Control | 2.00 (1.25; 3.00) |
| Main | 3.00 (2.00; 4.00) p = 0.001, p1 = 0.02, p2 = 0.001 | |
| Comparison 1 | 3.00 (2.00; 3.75) | |
| Comparison 2 | 2.00 (2.00; 3.00) | |
| Binucleari | Control | 2.00 (2.00; 3.00) |
| Main | 6.00 (5.00; 7.00) p = 0.001, p2 = 0.001 | |
| Comparison 1 | 6.00 (5.00; 7.00) p = 0.001 | |
| Comparison 2 | 3.00 (2.00; 3.00) | |
| Protrusions (broken egg, bubble) | Control | 1.00 (0.00; 1.00) |
| Main | 9.00 (8.00; 11.00) p = 0.001, p1 = 0.001, p2 = 0.001 | |
| Comparison 1 | 7.00 (6.00; 8.00) p = 0.001 | |
| Comparison 2 | 1.00 (1.00; 2.00) | |
| Cariorexis | Control | 4.00 (4.00; 5.00) |
| Main | 11.00 (9.75; 12.00) p = 0.001, p2 = 0.001 | |
| Comparison 1 | 11.00 (9.00; 12.00) p = 0001 | |
| Comparison 2 | 6.00 (5.00; 7.00) p = 0.001 | |
| Cariolysis | Control | 20.50 (18.00; 24.00) |
| Main | 33.00 (29.00; 36.00) p = 0.001 | |
| Comparison 1 | 32.00 (28.75; 37.00) p = 0.001 | |
| Comparison 2 | 33.00 (29.00; 38.00) p = 0.001 | |
| Vacuolization | Control | 9.00 (7.25; 10.75) |
| Main | 26.00 (24.00; 27.00) p = 0.001, p1 = 0.02, p2 = 0.001 | |
| Comparison 1 | 21.00 (19.00; 23.00) p = 0.001 | |
| Comparison 2 | 16.00 (14.00; 19.00) p = 0.001 |
Note: p – the level of significance of the probable difference in vs. the control, p1 and p2 – the level of significance of the probable difference vs. groups number 1 and number 2.
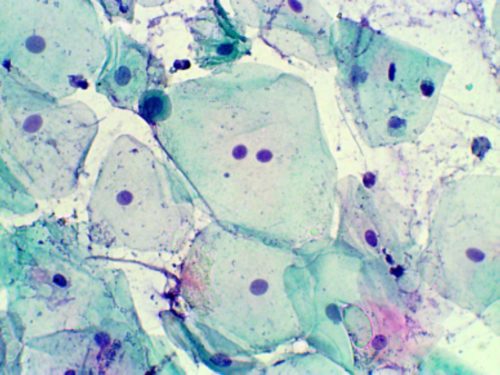
Binuclearity, is a common symptom of degenerative changes in the epithelium, and is characterized by the fact that two nuclei are in a single cell in the absence of the micronucleus. This change is most likely not due to damage to the nucleus, but due to membrane damage (peroxidation of cell membrane lipids) and cell loss of cytokinesis ability, that is, it reflects a certain energy deficit (Fig. 3).
Fig. 3. Microphotography of the patient’s gingival epithelium cytogramm. Binuclear epithelial cell is identified in the intermediate layer gingival mucosa. Staining by Papanicolau × 400.
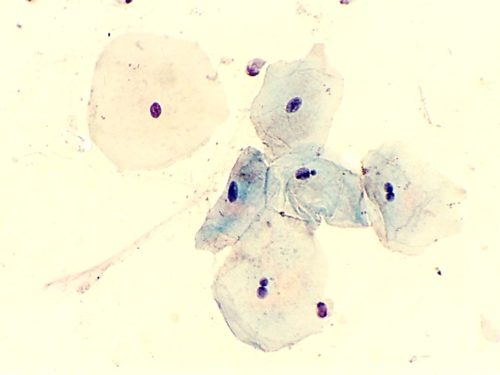
Parameter of genetic disturbances in the interphase nuclei may be the number of observed protrusions. The protrusion in the form of “broken egg” is represented by a micronucleus which is connected to the nucleus with a nucleoplasm bridge. The mechanism that leads to breach of the “broken egg” and “bubble” is not fully understood, but it is most likely associated with the elimination of amplified DNA or its residues.
Fig. 4. Microphotography of the patient’s gingival epithelium cytogramm. The epithelial cell with protrusions such as “broken egg” is determined. Staining by Papanicolau × 400.
The highest protrusion rate of the nucleus was also found in the main group, the incidence of which in patients with COPD with IHD is significantly increased and exceeded the control values by more than 9 (p < 0.001) times (Table 1).
In addition to cellular anomalies of the genetic nature in patients of all groups, according to the control group, gingival epithelium showed marked degenerative changes, manifested by the nucleus picnosis, violation of the integrity of the nuclear membrane, cariorexis and cariolysis. These changes are likely to be related to inflammation, but they can be a consequence and influence of medications taken by patients with regard to the underlying pathology. In COPD in combination with IHD, the incidence of such manifestations of inflammatory-destructive process in the epithelium as kariorexis (disintegration of the nucleus caused by chromatin aggregation) and caryolysis (partial or complete dissolution of the nucleus) is increasing.
Cariorexis is a degenerative change in the nucleus in a cell, accompanied by its disintegration into separate, intensely colored parts with a homogeneous structure, which after the lysis of the carriolems enter the cytoplasm and undergo resorption.
Morphologically, cariorexis is a cell with several large or numerous small, stained nucleus fragments in the cytoplasm. Cariolysis is a degenerative change in the nucleus in a cell that is accompanied by a loss of chromatin staining ability, followed by its complete disappearance.
Morphologically, it is a cell with a homogeneous staining on of the nucleus and a fuzzy decaying cacyolemma (early stage of cariolysis) or a cell with a complete lack of coloration of the nucleus, when it has the form of a shadow on the background of the stained cytoplasm (full stage of cariolysis).
According to Table 1, in all of the study groups, besides the group of somatic healthy patients, there was a probable increase in the degenerative anomalies of the nucleus.
Fig. 5. Microphotography of the patient’s gingival epithelium cytogramm. The accumulation of epithelial cells in the surface of the gingiva with the presence of perinuclear halo and signs of vacuolization is determined. Staining by Papanicolau × 400.
In COPD and IHD, hypoxia, microcirculation and vascular permeability and increased lipid peroxidation may contribute to this. The above-mentioned violations are likely to result in an increase in the number of cells in the epithelium of patients with increased vacuolization, which is a sign of early cell destruction, in particular destructive changes in cell membranes and a decrease in their barrier and transport function.
With pronounced vacuolization the cytoplasm can be preserved only in the peripheral cell department, forming a perinuclear halo (around the nuclear zone of enlightenment, formed due to degenerative changes and necrosis of the destroyed cytoplasmic organelles).
Conclusions. The results of the conducted study indicate that the most pronounced changes in the cell nucleus are inherent in patients with mixed broncho-cardial pathology. Intracellular re-organization of gingival epithelium in examined patients has stereotypical manifestations, typical for chronic inflammation. Thus, we can speak about the presence of genotoxic effects of a somatic disease or its treatment on the manifestation of cellular anomalies of gingival epithelium in patients with COPD in combination with IHD.
References
- Van der Biel P. Interrelation of periodontal diseases and cardiovascular system. Problems of Stomatology. 2014;6:4-8. (Russian)
- Grigoryan AS, Rabukhina NA, Grudyanov AI, Frolova OA. Problems of diagnostics of early phases of inflammatory periodontal diseases. New in Dentistry. 2001;8:3-8. (Russian)
- Gurevich MA, Dolgova EV, Kuzmenko NA. Chronic obstructive pulmonary diseases, arterial hypertension and ischemic heart disease: features of pathogenesis, clinical picture, therapy. Russian Medical Journal. 2016;16:1098-1102. (Russian)
- Ismoilov AA, Amurov GG. Results of the evaluation of the condition of periodontal tissues in patients with obscheomatic pathology. Scientific and Practical Journal of IPGEMS. 2012;4:4-12. (Russian)
- Pervov YuYu, Gurbanov KR, Bolotnaya VN, Popova KM, Ignatiev SA, Pogorely VV. Cytological indicators as an assessment of the condition of periodontal tissues in prosthetic patients with diabetes mellitus. Fundamental research. 2007;11:68-69. (Russian)
- Romanenko IG, Poleshchuk OYu, Kaladze KN. The state of hygiene of the oral cavity and periodontal tissues in children with chronic generalized catarrhal gingivitis on the background of bronchial asthma. News of problems of biology and medicine. 2014;2(2):121-125. (Russian)
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (GOLD): Updated 2016. 80 p.
- Shen TC, Chang PY, Lin CL, Chen CH, Tu CY et al. Risk of periodontal diseases in patients with chronic obstructive pulmonary disease: a nationwide population-based cohort study. Medicine (Baltimore). 2015;94(46):e2047. https://doi.org/10.1097/MD.0000000000002047
- Tonetti MS, Van Dyke TE. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/ AAP Workshop on Periodontitis and Systemic Diseases. J Periodontol. 2013;84 (4 Suppl):24-29. https://doi.org/10.1111/jcpe.12089
- Zeng XT, Tu ML, Liu DY, Zheng D, Zhang J, Leng W. Periodontal disease and risk of chronic obstructive pulmonary disease: a meta-analysis of observational studies. PLoS One. 2012;7:46508. https://doi.org/10.1371/journal.pone.0046508